AI-Powered Prior Authorization Management Solution
Designed by clinicians for clinicians, Banjo Health’s user-friendly solution increases efficiency and effectiveness across your teams.
%20(1).gif)
Our Customers





















Solution Overview

End-to-end case management solution for prior authorizations and appeals.

Prior Authorization Workflows
Leverage AI to streamline the process, reduce administrative burden, and improve decision-making speed.

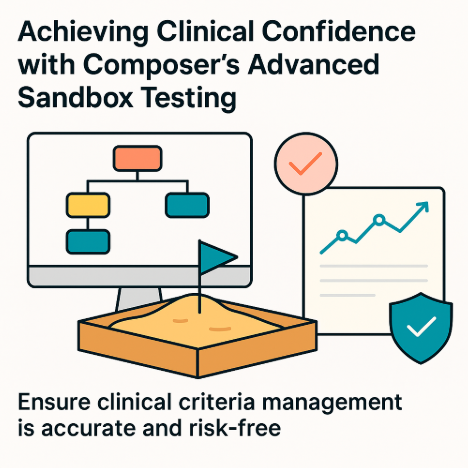
Clinical Decision Tree Generator
Transform complicated clinical criteria into actionable, electronic decision trees within seconds, improving speed and accuracy.
.svg)
Appeals & Grievances Tool
Efficiently manage appeals and grievances with speed and compassion to deliver a better member experience.
Enterprise Prior Authorization Management

Our mission is to make healthcare simpler.
See Banjo Health in action.
Take a look at our latest articles and resources
Frequently Asked Questions
Banjo Health empowers health plans and PBMs with AI-driven software that simplifies and accelerates Prior Authorizations, Appeals, Grievances, and Clinical Criteria Automation. Our solutions are designed to reduce costs, enhance operational efficiency, and improve patient care outcomes.
By automating complex workflows, Banjo Health delivers faster, more accurate results for patients and providers alike. Tools like BanjoPA, BanjoAppeals, BanjoGrievances, and Composer streamline processes, enabling real-time decision-making, productivity gains, and meaningful cost savings.
Our adaptable, no-code platform integrates seamlessly with existing systems, supporting real-time case management, automated compliance, and intelligent insights that continuously evolve with your organization’s needs. With Banjo Health, healthcare organizations gain the responsiveness and innovation required to stay ahead in today’s dynamic environment.
Banjo Health leverages advanced Artificial Intelligence (AI) to transform the prior authorization (PA) process, streamlining workflows, improving compliance, and enabling faster, more accurate decisions. By integrating tools like Composer and CARE (Computer Assisted Review Engine), our AI-powered platform automates complex processes while continuously learning and adapting to evolving clinical and regulatory requirements.
Banjo Health provides a comprehensive suite of tools designed to streamline prior authorizations, appeals, and grievances. BanjoPA automates end-to-end prior authorization workflows, ensuring efficiency and accuracy. Composer simplifies the integration of clinical criteria by converting them into decision trees that seamlessly fit into workflows. Banjo Appeals and Grievances centralize case management, enabling compliance and faster resolutions for a more effective appeals process.
Banjo Health stands out with purpose-built AI models designed specifically for prior authorizations. Our solutions are fully customizable, integrate seamlessly with existing systems, and continuously learn and adapt to evolving clinical and regulatory requirements.
Yes, Banjo Health’s platform is designed for seamless integration with EHRs, eligibility verification tools, claims management systems, and more. Our flexible, API-supported infrastructure ensures all relevant data flows smoothly between systems, reducing duplication and improving efficiency.